For three decades, the Endoscopy Center in the Division of Gastroenterology, Hepatology and Endoscopy at Brigham and Women’s Hospital has been pioneering advanced endoscopic techniques.
For three decades, the Endoscopy Center in the Division of Gastroenterology, Hepatology and Endoscopy at Brigham and Women’s Hospital has been pioneering advanced endoscopic techniques.
Since 2012, Christopher C. Thompson, MD, MSc, an interventional gastroenterologist and director of Endoscopy at the Brigham, and his team of interventional endoscopists have been developing novel uses for lumen-apposing metal stents (LAMS). These stents are dumbbell-shaped with wide-bore saddle regions that are short in length.
Developing New Ways to Use LAMS Beyond Pancreatic Fluid Collection (PFC)
The Brigham team uses the AXIOS™ Stent and Electrocautery Enhanced Delivery System, which was approved by the U.S. Food & Drug Administration (FDA) in 2013 to manage peripancreatic fluid collections (PFCs). While LAMS are most commonly used for PFCs, these stents are increasingly being used for various other off-label indications.
“The Brigham has had access to LAMS longer than most centers, so we started using them beyond PFCs with a focus on making procedures more efficient and less invasive. For the last seven years, the Endoscopy Center has been leading the way in developing innovative endoscopic procedures using this technology,” says Dr. Thompson.
Currently, the Brigham’s Interventional Endoscopy Group is using LAMS in several innovative ways. These include: performing endoscopic retrograde cholangiopancreatography (ERCP) in patients with gastric bypass anatomy; gastroenterostomy for palliation of malignant gastric outlet obstruction; and endoscopic ultrasound (EUS)-guided drainage of the gallbladder for cholecystitis.
Using LAMS in Patients with Roux-en-Y Gastric Bypass (RYGB) Anatomy
An increasingly common procedure in patients who have undergone Roux-en-Y gastric bypass (RYGB) is ERCP. However, ERCP and other foregut procedures have been technically challenging in these patients.
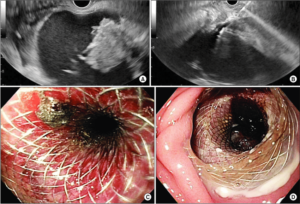
In a 2019 paper in Surgical Endoscopy, Dr. Thompson and Marvin Ryou, MD, director of Endoscopic Innovations at the Brigham, in collaboration with Thomas Wang, MD, developed a new approach to ERCP and other endoscopic foregut procedures in 10 patients with gastric bypass anatomy. The procedure, which uses LAMS, is an optimized version of the EUS-directed transgastric ERCP (EDGE) that the authors termed gastric access temporary for endoscopy (GATE).
 The GATE procedure allows Brigham’s interventional endoscopists to provide standard of care endoscopic assessment and treatment in patients with surgically altered anatomy, particularly in patients with RYGB anatomy. In their study, Drs. Thompson and Ryou demonstrated methods for safely opening and closing the access track as well as restoring the original anatomy following the GATE procedure.
The GATE procedure allows Brigham’s interventional endoscopists to provide standard of care endoscopic assessment and treatment in patients with surgically altered anatomy, particularly in patients with RYGB anatomy. In their study, Drs. Thompson and Ryou demonstrated methods for safely opening and closing the access track as well as restoring the original anatomy following the GATE procedure.
“The GATE procedure involves EUS-guided creation of a temporary access tract using LAMS. The temporary access between the remnant stomach and the gastric pouch allows us to re-establish continuity of the stomach. We can then drive endoscopes through the temporary access to perform foregut procedures,” says Dr. Ryou.
In addition to ERCP, GATE also facilitates endoscopic procedures of the foregut in patients who have undergone EUS and endoscopic submucosal dissection (ESD). The Endoscopy Center also regularly performs GATE to remove gallstones in patients with RYGB anatomy.
“We are now working on a cost-utility analysis of GATE, comparing it with historical methods to assess its cost effectiveness. Compared to other methods, results of this investigation show that GATE is less expensive to the health care system,” says Dr. Ryou.
LAMS for Gastric Outlet Obstruction
In addition to GATE, the Interventional Endoscopy Group at the Brigham is using LAMS to perform gastro-enteral anastomoses in patients with cancer and gastric outlet obstruction. Using LAMS, Dr. Thompson and his team can connect the stomach to the small bowel just beyond the area of obstruction.
In a 2019 study in Surgical Endoscopy, Dr. Thompson and colleagues demonstrated that gastroenterostomies created by the LAMS provided more effective palliation with a lower re-intervention rate compared to enteral stents. Patients also had better symptom control and efficacy.
“We use LAMS to bypass the area of cancer, allowing food to go from the stomach directly into the small bowel,” explains Dr. Thompson. “This offers advantages over traditional stenting, which involves placing a stent across the tumor. The problem with this traditional method is that tumor overgrowth or ingrowth can lead to early stent occlusion, and many patients have to return for additional procedures.”
Using LAMS is now the Endoscopy Center’s preferred approach for treating gastric outlet obstruction. Oncologists have been sending Dr. Thompson and Dr. Ryou patients to treat gastric outlet obstruction specifically requesting this novel procedure.
EUS-guided LAMS Drainage of the Gallbladder
The Endoscopy Center has also been performing EUS-guided gallbladder drainage using LAMS in patients with cholecystitis who would otherwise require a percutaneous drain. Studies show that internal drainage using LAMS is safe and provides better palliation with a lower need for re-intervention, compared to external drainage.
In collaboration with Drs. Thompson and Ryou, Thomas McCarty, MD, a research fellow in the Department of Gastroenterology, Hepatology, and Endoscopy, recently completed a cost-effectiveness analysis demonstrating the advantages of this technique compared to external catheter drainage.
“Percutaneous drainage is unpleasant for patients and is associated with a relatively high rate of re-intervention due to catheter dislodgement or other adverse events. Our method of internal drainage has several advantages, including the ability to remove purulent, viscous fluid, sludge and stones,” says Dr. Thompson.
A Culture of Innovative Endoscopy at the Brigham
“The innovative ways that we are using LAMS is an example of how the Brigham is paving the way in endoscopic surgery. We’re making endoscopy more surgical in nature, creating more effective and less-invasive alternatives for patients,” says Dr. Thompson.
Going forward, Dr. Thompson hopes that these novel LAMS procedures will be more broadly adopted to positively impact the care of patients with a variety of conditions.