Natalie Artzi, PhD, a principal investigator in the Brigham and Women’s Hospital Department of Medicine, has changed our basic understanding of biomaterials under different environmental and pathological states. Her laboratory is dedicated to designing smart biomaterial platforms and medical devices to improve human health.
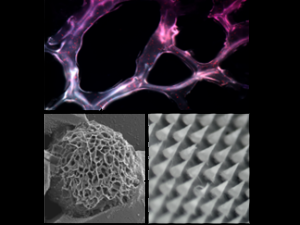
In a presentation at the 2023 Mass General Brigham Gene and Cell Therapy Research Symposium, Dr. Artzi presented her work on the use of nanostructures in drug delivery, immune therapy, and gene therapy. Her lab has generated a library of nanomaterials based on polymeric and lipidic structures that deliver a wide range of therapeutics for various diseases as well as devices—from adhesive hydrogels to “smart Band-Aids.”
“Nanostructures are particularly useful in shuttling drugs to target tissues in the context of systemic diseases,” Dr. Artzi says. “But in many cases, overcoming biological barriers to delivery can benefit from local and sustained delivery of these nanostructures from biomaterial depots that can be injected or sprayed directly to the target site.
“A good example is local delivery in the brain that eliminates the need to cross the blood-brain barrier. Engineering biomaterials to overcome barriers to the controlled spatiotemporal distribution of immunotherapies and enabling their subsequent combination with existing and novel therapeutic modalities can further revolutionize cancer care.”
Nanoparticles Train the Immune System to Target Cancer Cells
According to Dr. Artzi, one of the most exciting uses of nanoparticles is for interaction with the immune system. For instance, in cancer therapy, nanostructures can be leveraged to train the body’s immune system to identify and then eliminate cancer cells by creating an anti-tumor immune memory, akin to the way a vaccine works.
“Cancer cells exist in the tumor microenvironment, but immune responses and reactions also happen in other organs, like the lymph nodes, spleen, and bone marrow,” she says. “Nanomaterials that are stable and can efficiently load and protect drug cargos can be used to enhance our understanding of what tissues and cells contribute to the generation of anti-tumor immune responses.”
Dr. Artzi and her laboratory colleagues studied the role of the cGAS-STING pathway—a conserved pathway in the body that gets activated in response to an infection—in delivering a Takeda STING agonist drug via nanostructures. They found success in a cyclic dinucleotide (CDN) conjugated nanoparticle, which maintains high activity and good activation in reporter cells, dendritic cells, and macrophages in mouse models.
Dr. Artzi and her team discovered that when CDN-conjugated nanoparticles were combined with an anti-PD1 checkpoint blockade, tumor cells were better eliminated, resulting in a 60% were able to activate dendritic cells that present tumor antigens to T cells that in turn become cytotoxic and eliminate cancer cells; we increase the number of, and activate, natural killer cells and polarize macrophages. All of these together contribute to tumor elimination and antitumor immune memory formation,” she says.
Taking the next step, the team rechallenged the cured mice after 60 days without treatment. Approximately 70% of those mice rejected the tumor, pointing at a successful anti-tumor memory formation. In a similar test of mice with colon cancer, 100% rejected the tumor.
Shifting Focus to the Spleen
Dr. Artzi’s work revealed the players contributing to memory (the ability to train the immune system to generate anti-tumor response), prompting her to investigate the biodistribution of nanoparticles and anti-tumor cell activation in the spleen. She studied splenectomized mice and wild-type mice, finding they both had the same treatment response in eliminating the primary tumor. However, when cured mice were rechallenged, the wild-type mice could reject the tumor, while splenectomized mice could not.
“That was, in part, a result of splenectomized mice having fewer lymphocytes that can be educated to eliminate the tumor and generate memory,” she says. “Leveraging our nanostructures to generate stable and potent nanomedicines, we can enhance the therapeutic window and enable studying drug mechanisms of action.”
Microneedling: A Better Way to traverse drugs through the skin
Dr. Artzi’s lab developed a microneedle patch that can deliver drugs effectively across the skin, as well as sample biomarkers in skin interstitial fluid noninvasively. The ability to deliver drugs where needed, for example in the treatment of melanoma and autoimmune skin diseases, enables enhancing therapeutic outcomes while eliminating side effects associated with the systemic delivery of the drugs. In her work, Dr. Artzi shows that the delivery of factors that can recruit and expand regulatory T cells to lesions in the skin, such as bold areas in alopecia areta, enables restoring immune homeostasis and induce tolerance. Similarly, in a melanoma model the patch enabled delivery of immune modulators to activate the immune system to eliminate the cancer, as well as sample cellular and soluble biomarkers that report on the response to the therapy longitudinally and noninvasively.
“The ability to design devices and engineer nanostructures that can help protect and shuttle drugs to its target can serve as a tool to interrogate immunological responses across biological scales and inform on the optimal choice, regimen, and duration of therapy,” she says.