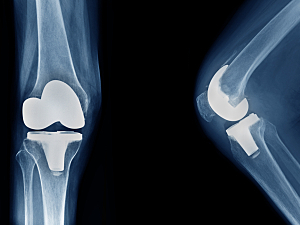
Total Joint Arthroplasty: Should Patients Stay or Should They Go?

Historically an inpatient procedure, total joint arthroplasties (TJAs) were recently removed from the U.S. Centers for Medicare & Medicaid Services’ inpatient-only list. Now the Brigham is leading the trend toward same-day discharge TJAs. Antonia F. Chen, MD, MBA, explains how the Brigham is managing this transition.
Read More...