Cumulative Incidence Curves of the Composite Endpoint of MI or Stroke
Cardiovascular Risks of Probenecid Versus Allopurinol in Older Patients with Gout. Seoyoung C. Kim, Tuhina Neogi, Eun Ha Kang, Jun Liu, Rishi J. Desai, MaryAnn Zhang, Daniel H. Solomon. Journal of the American College of Cardiology Mar 2018, 71 (9) 994-1004; DOI: 10.1016/j.jacc.2017.12.052
Inflammation plays a critical role in the pathogenesis of both gout and cardiovascular disease (CVD). It is well known that patients with gout are at an increased risk of CVD, including myocardial infarction (MI), stroke, and heart failure (HF). While it remains controversial whether uric acid is causally linked to the development of CVD, beneficial effects have been reported for allopurinol, the most commonly used urate-lowering drug, on lowering blood pressure and improving endothelial function and metabolic profile. Probenecid is another, older drug used for gout. It works as a competitive inhibitor of the organic anion transporter, producing uricosuria, as well as an inhibitor of pannexin 1 channels, an ATP release channel involved in the assembly and activation of the inflammasome. The NLRP3 inflammasome plays a critical role in production of IL-1β, which drives the inflammatory cascade that results in acute gout. Thus, it is possible that probenecid may have positive effect in gout patients not only by lowering serum urate levels, but also by reducing production of IL-1β.
Read More


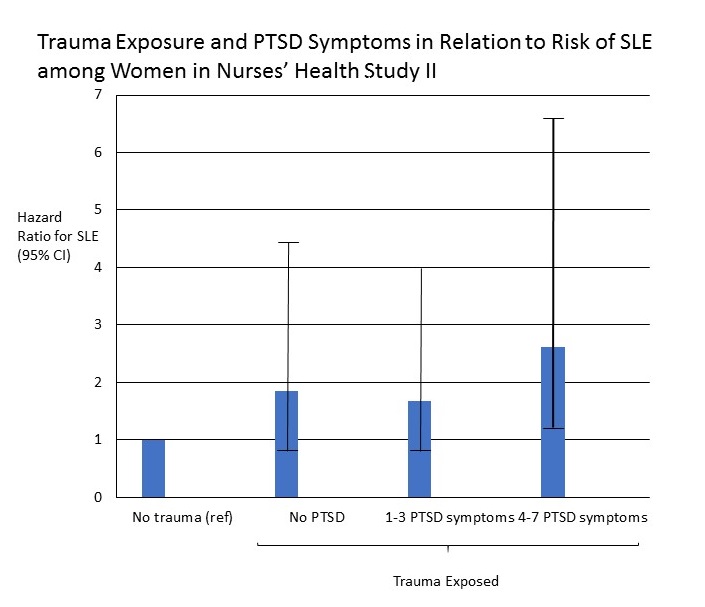 Andrea L. Roberts, PhD, Susan Malspeis, MS, Laura D. Kubzansky, PhD, Candace H. Feldman, MD, Shun-Chiao Chang, ScD, Karestan C. Koenen, PhD, Karen H. Costenbader, MD, MPH Arthritis & Rheumatology, 2017;69(11):2162-2169.
Andrea L. Roberts, PhD, Susan Malspeis, MS, Laura D. Kubzansky, PhD, Candace H. Feldman, MD, Shun-Chiao Chang, ScD, Karestan C. Koenen, PhD, Karen H. Costenbader, MD, MPH Arthritis & Rheumatology, 2017;69(11):2162-2169.